Living with COPD
Sections in this leaflet
About the Team
Call 01865 904418 Mon-Fri 08.30-16.30
The team aim to support people to manage their COPD and try to avoid the need for hospital admissions when having exacerbations.
We are a large, county wide team with a number of components of the service.
We have a team in Banbury who see patients in the community as well as in-reach to the Horton hospital to support early discharge where possible, and another team based at the John Radcliffe who do the same in Oxford.
The community team have caseloads covering different geographical areas across Oxfordshire, visiting people at home to optimise their COPD management, and ensuring people have a good understanding of what to do if they become unwell with their breathing.
The team will offer home visits after any hospital admission and will also support if you have a flare up (exacerbation at home).
We have several clinicians who provide a Home Oxygen Assessment and Review Service, these clinicians will assess for appropriate oxygen prescription and equipment to help manage long standing low oxygen levels.
The teams have clinics, and where needed, a domiciliary service.
Part of the team run the Pulmonary Rehabilitation service: This is an 8-week exercise and education program, that runs twice a week.
It is designed for people with lung disease who are limited by symptoms of breathlessness.
These classes are run face to face at venues around the county and virtually online.
The team links in with your GP and practice nurse, as well as hospital doctors at The John Radcliffe.
We have a duty clinician every day who is available to speak with you if you have any concerns about your breathing.
You call will be triaged by our administrators, so please give enough detail for us to know the nature of your call.
The Duty clinician will then call you back during the day. Please do not hesitate to call us for support / advice.
You may need to leave a message, and we will call you back.
What is COPD?
Chronic
It’s a long-term condition and does not go away.
Obstructive
Your airways are narrowed so it is harder to breath out quickly.
Pulmonary
It affects your lungs.
Disease
It’s a medical condition.
Understanding the airways
These diagrams illustrate the lungs and airways within the lungs when they are healthy and when they are damaged with COPD.
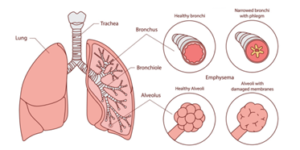
Diagram of the lungs
Signs you may have a flare up (exacerbation or attack)
A flare up, (sometimes called an exacerbation or an attack) is when your symptoms increase and can become particularly severe over a period of time; less than 14 days (GOLD 2023).
This might be triggered by an infection or there may be no apparent reason you can identify.
- It is very important to recognise symptoms early and start treatment to avoid becoming unwell. Please see your Action Plan on the following page as advised by your Health Care Professional.
Common signs are
- Increased feeling of more breathless than usual at rest and when moving about.
- Coughing more and producing more sputum than usual.
- Your sputum may also change in colour and consistency. Change in colour to Yellow or green might indicate you have an infection.
- Changes in the volume of your sputum even if it has not changed colour can suggest this too.
- You may develop a wheeze or chest tightness
What can you do?
If you have one of these symptoms using your reliever (usually salbutamol) inhaler, through the spacer, 2-4 single doses up to 4 times a day may help.
If you are very breathless -Take one puff of your reliever inhaler (usually blue) with the spacer every 30-60 seconds up to 10 puffs.
If you have a Pulse Oximeter (finger probe), record your oxygen saturations at rest. Remember to rest for 15-20 minutes and ensure your hands are warm and still when you take the reading.
It’s important to know your usual level when you are well to compare.
Use you Lung monitor (if you have been given one) to record any changes and let the team know both these readings.
Your action plan
Take your usual inhaler puffs a day
Increase your inhaler to puffs a day (via a spacer)
Your nebuliser solution is:
Chest clearance:
Antibiotics:
start these when you are producing more phlegm (mucus) than usual or it has changed colour, as well as being more breathless for some time despite taking reliever medication
Steroids:
These should be started if you are more breathless than usual despite increasing your reliever inhaler.
If you need courses of steroids more than twice a year you should be reviewed by your GP or specialist.
When you are unwell with your breathing
Tell your GP practice when you start taking your rescue pack
Most flare ups can be treated at home but if you need any advice or support call you respiratory practitioner.
Sometimes people need to go to hospital. If you use the ambulance service, be sure to tell them you have COPD so that you get the right oxygen treatment.
Seek urgent medical advice if:
- Your breathing is not improving
- You cough up blood
- You notice any new or worsening ankle swelling that does not go down overnight
- You get new chest pain
- If you are more confused, drowsier or generally feel you cannot cope with the flare up alone
It can take up to 8 weeks to recover from a flare up of COPD.
Seeking additional help
You can ask your pharmacist if you require advice. You can have a telephone appointment with your GP. If they need to see you, they will ask you to attend the surgery.
If you need help fast you can go to NHS 111 by phone or online. They may arrange for you to see a doctor or attend a walk-in centre.
If your breathing is much worse and you require urgent help call 999
Keeping Healthy
Exercise
Regular exercise is important to improve the condition of your lungs and it can benefit your wellbeing and enjoyment of life.
People with breathing difficulties sometimes avoid exercises as it can cause breathlessness.
It is not actually harmful if the exercise is introduced gradually and sensibly.
Pulmonary Rehabilitation teaches you how to exercise at the right level for you and helps you understand how to manage your condition. It can also benefit your health and wellbeing.
Often, people with moderate to severe breathing problems see the greatest benefit from pulmonary rehabilitation.
Speak to the Team for more details.
Be careful what you breathe
It is important for your health to stop smoking and to avoid smoky places.
For help and advice with this call
Stop for Life: 08001223790
Website: https://www.stopforlifeoxon.org
Avoid dust by damp dusting and open windows when dusting or vacuuming.
Open windows if using strong smelling cleaners and avoid plug-in or spray air fresheners or candles.
Wear a mask if you are going to do something that creates a lot of dust, for example cleaning out pets’ cages, decorating, or sanding wood.
Try to avoid people with coughs and colds – you could wear a mask to avoid catching any colds or viruses.
Medication
Take all your prescribed medication, especially your inhalers as they are prescribed. Check with the team you are taking them correctly and speak to your nurse or doctor if you are unsure what to take.
Inhaler disposal: all empty inhalers should be returned to Pharmacies for safe disposal. This reduces the risk of harmful gases being released into the environment if they are thrown away in the normal rubbish.
Vaccinations
Having vaccinations for influenza flu, coronavirus and pneumococcal vaccines will reduce your risk of becoming seriously ill if you come into contact with viruses.
You may feel unwell for a few days after the vaccinations whilst your immune system is activated, rest and regular paracetamol can help with any symptoms.
Breathlessness
Using a handheld fan and breathing control techniques such as rectangular breathing can help when you are breathless.
To do this, follow the shape of a rectangle with your eyes: take a short breath in (short side of the rectangle) and a longer breath out (longer side of the rectangle).
Continue with this breathing
Also try the 4 Fs
- Fan
- Focus on breathing out
- Forward leaning
- Flop the shoulders
Refer to our Managing Breathlessness booklet for more information.
Airway secretions
Some people have problems with clearing their airway secretions.
If this is a problem for you, it is important to complete airway clearance techniques regularly.
Having regular sips to drink can help with this, including fresh pineapple (juice or fruit).
Ensure you are taking the correct dose of carbocisteine if you are prescribed this (ask our team).
Speak to your clinician if you need more advice and ask for an Active Cycle of Breathing leaflet.
Coping with the weather
Hot or dry days
Use fans, stay hydrated, keep cool, and avoid areas with lots of dust or fumes.
Cold or damp days
Avoid being outdoors when it is misty and damp.
Keep warm, wear a warm coat, hat, gloves, scarf when outdoors and keep your house warm.
A mask or scarf loosely wrapped around your face is a good way to keep the air you breathe in warm.
Keep warm
In the winter it is important to keep warm inside and outdoors.
This can help stop you getting colds, flu and more serious health problems.
Heat your home, or at least the room you are sitting in, to a minimum of 18 degrees centigrade (65F).
Keep your bedroom window closed on cold nights so that you do not breathe in cold air.
Move around indoors at least hourly.
Wear lots of layers of thin clothes
Have regular warm drinks.
Find out how you could pay less to heat your home at www.simpleenergyadvice.org.uk or call 0800 444202 or talk to your local citizens advice.
Better Housing, Better health contact 0800 1070044
Be prepared
Try to ensure you order your inhalers and medicines in good time and do not run out, especially on weekends and Bank holidays.
Keep enough food in the house for a few days in case of bad weather (hot or cold).
If you have to go out wear shoes with a good grip and wrap a scarf over your nose and mouth so that you are not breathing in cold air, If you are able, wear a mask when you go out shopping.
Let someone know if you are unwell so that they can keep a check on you; if relatives have coughs and colds, ask them to stay away.
Nutrition
Eat a balanced diet with plenty of fruits and vegetables.
If eating makes you breathless, try to eat smaller meals more often, sit at a table, and use oxygen if you are prescribed it.
Make sure you are well hydrated. Aim for 2 litres daily (preferably water and decaffeinated drinks) unless you are on a fluid restriction.
Speak to your GP if you are losing weight unintentionally.
Handwashing
Washing your hands with soap and water is one way of reducing your risk of getting illnesses like flu and coronavirus.
Wash your hands for 20 seconds especially:
- When you have been out
- After you blow your nose, sneeze or cough into a tissue
- Before you eat or touch food or medicines
- After you have been to the toilet
The challenges of living with COPD
People with COPD can have restricted mobility, breathlessness, and a decrease in their quality of life.
It is often more difficult to go out, they can be more dependent on others, and this can be difficult.
For this reason, they can be up to three times more likely to experience anxiety and/or depression which further impacts their home and work life.
You can talk to your clinician about this, and Talking Therapies have specifically trained staff to provide talking therapies for people living with COPD who are experiencing feelings of depression and/or anxiety.
You can self-refer to this service.
Telephone: 01865 901222
Website: www.talkingspaceplus.org.uk
In writing: Talking Therapies, Abell House, The Slade, Horspath Driftway, Headington, Oxford, OX3 7JH
Support groups
We run a COPD peer support group in Marston, Oxford on alternate Wednesdays 12-1pm.
It is an informal opportunity to meet others with COPD and have a complimentary tea or coffee. Everyone is welcome. For more details call the team.
There is a Breathe Easy Group in Banbury which meets on the first Monday of the month.
They meet at The Army Reserve Centre, 5 Squadron, Oxford Rd, Banbury OX16 9AN. Contact Jenny 07813448257 banburybreatheeasyclub@gmail.com
Social care
If you or your family have additional care, equipment needs or are struggling financially call –
Oxfordshire County Council Adult Social Care: 03450507666 or go to their website oxfordshire.gov.uk
Food poverty
It is important for your health and wellbeing that you eat at least one hot meal each day. Thick, warm soups are nutritious and can help keep you fuller for longer.
If you are struggling to buy food you should let someone know, you can always talk to a member of our team.
Other useful contacts
Asthma and Lung health Helpline: 03002225800 9am-5pm weekdays Website www.asthmaandlung.org.uk
Single Point of access (Patient line) 01865 903750
Move Together organisation that can provide advice, motivation and signposting to a variety of activities for you to try. Visit getoxfordshireactive.org/move-together
Silverline https://www.thesilverline.org.uk 08004708090 Call for conversation, friendship and support.
No matter who you are, how your day is or what’s going on in your life, everyone needs someone to talk to. Call free and confidentially any day of the year, at any time. Open 24 hours a day, every day.
Age UK: 08006781602 open 8am-7pm everyday
Carers Oxfordshire: 01235 424715
PALS: Oxford Health NHS Foundation Trust aims to provide high quality care and services for our patients but sometimes we don’t get it right.
PALS can help you with support and advice, support to sort out a local concern or problem quickly, the opportunity to make a compliment, comment or suggestion to improve services and help with raising a formal complaint.
contact details 08003287971 email PALS@oxfordhealth.nhs.uk website oxfordhealth.nhs.uk
Service available weekday 9.30-4.30 (24 hour answerphone)
General guidance: Contact us
Oxford Health NHS Foundation Trust, Trust Headquarters,
Littlemore Mental Health Centre, Sandford Road, Littlemore, Oxford OX4 4XN
- Switchboard: 01865 901 000
- Email: enquiries@oxfordhealth.nhs.uk
- Website: www.oxfordhealth.nhs.uk
Become a member of our Foundation Trust: www.ohftnhs.uk/membership
Page last reviewed: 20 December, 2024
